Cell therapy is a medical procedure that involves introducing cellular material into a patient. The cells can either be from the patient themselves (autologous) or from another donor (allogeneic).
Cell therapy practices have their roots tracing back to the 19th century and have since evolved significantly with increasing research and investment. Cell therapy encompasses a wide range of treatments, including stem cell therapy, non-stem cell therapy, single-cell and multi-cell therapies. These therapies exhibit distinct immunophenotypic profiles, isolation methods, mechanisms of action, and levels of regulatory oversight. In line with the footsteps of earlier established or commercialized cell therapies, experimental and premarket approval-exempt cell therapies continue to offer promising therapeutic advantages to patients across various disease areas. The concept of cell therapy has been around since the late 1800s, and it continues to evolve today with ongoing research to ensure its safety and effectiveness. The global market for cell therapy is expected to grow significantly from USD 9.5 billion in 2021 to an estimated USD 23.0 billion in 2028.
Currently, two distinct categories of cell therapy exist. The first falls within mainstream medicine and includes allogeneic cell therapy, human embryonic stem cell therapy, neural stem cell therapy, mesenchymal stem cell therapy, and hematopoietic stem cell therapy. These therapies are the subject of extensive research and hold great promise for therapeutic benefits. Research in this category, particularly when involving human embryonic materials, can be contentious. The second category belongs to alternative medicine and involves the injection of animal materials in an attempt to cure diseases. However, this practice lacks medical evidence of effectiveness and can even have harmful consequences, as noted by the American Cancer Society.
Cell therapy can involve different types of cells, including stem cells or non-stem cells. The cells can be administered in various ways, such as through injections, infusions, or topical applications. This diverse field is used in multiple medical areas, including regenerative medicine, immunotherapy, and cancer treatment.
Clinical Benefits of Cell Therapy
Cancer
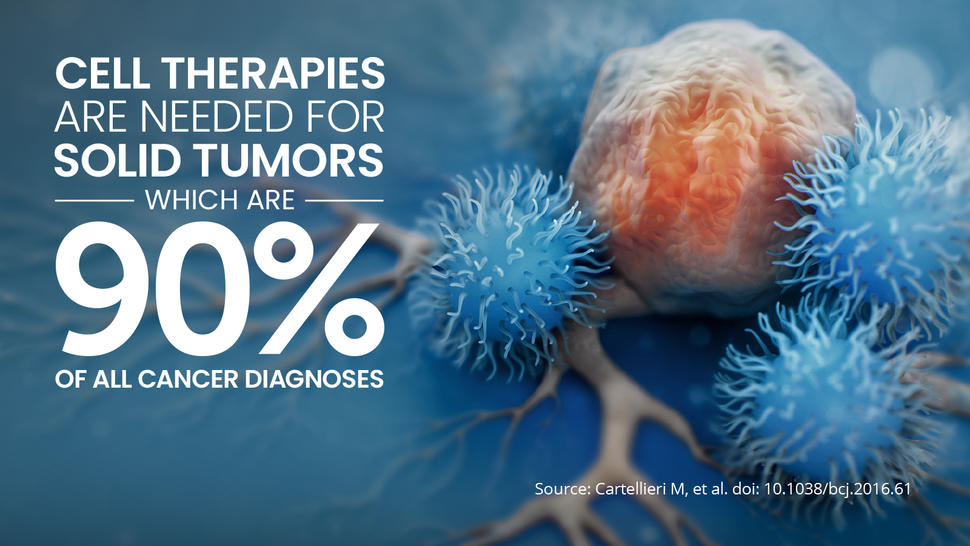
Cancer therapy strategies have evolved over time, transitioning from broad systemic treatments like chemotherapy and radiotherapy to more precise approaches utilizing novel biological therapies. These advanced treatments include monoclonal antibodies, oncolytic viruses, and cell-based therapies such as antigen-presenting cell (APC)-based anticancer vaccines and CAR-T cells. Hematological malignancies, in particular, have seen significant advancements in the regeneration of immune effectors, with Hematopoietic Stem Cell Transplantation (HSCT) being a standard treatment.
In 2010, PROVENGE® (sipuleucel-T) received FDA approval as the first APC-based anticancer vaccine, primarily for treating metastatic castration-resistant prostate cancer. Later in 2017, KYMRIAH™ (tisagenlecleucel) became the inaugural CAR-T cell therapy to gain FDA approval, specifically for the treatment of relapsed or refractory B-cell precursor acute lymphoblastic leukemia and large B-cell lymphoma. Subsequently, other autologous CAR-T cell therapies directed at CD19 entered the market for the treatment of relapsed or refractory large B-cell lymphoma or mantle cell lymphoma. In 2021, ABECMA® (idecabtagene vicleucel) became the first CAR-T cell therapy targeting B-cell maturation antigen (BCMA) to receive FDA approval for the treatment of relapsed or refractory large B-cell lymphoma.
Apart from these commercially available cell therapies, numerous investigational cell therapies have been explored in clinical settings for cancer treatment. Among APC-based anticancer vaccines, DC-based vaccines, whether generated with primary CD1c+ myeloid DCs or engineered by fusion with patient-derived tumor cells, have shown promise in B-cell lymphoma, multiple myeloma, acute myeloid leukemia, glioblastoma, and metastatic melanoma. CD34+ HSC-derived modified/manipulated DCs have also yielded positive outcomes, including the generation of tumor-specific immunity and induction of tumor regression in metastatic melanoma patients. The fusion of autologous primary DCs with irradiated tumor cells followed by bioengineering and administration to glioblastoma patients undergoing standard chemotherapy has improved clinical responses. Additionally, vaccination of acute myeloid leukemia patients in remission using autologous primary DCs fused with autologous cancer cells has expanded tumor-reactive T cell subsets and prolonged remission.
Investigational CAR-T cells have demonstrated significant antitumor activity in relapsed/refractory multiple myeloma by targeting BCMA. However, CAR-T cells directed against solid tumor antigens like PD-L1 and prostate-specific membrane antigen (PSMA) have faced challenges in the suppressive tumor microenvironment and therapy persistence within the tumor. Bispecific CAR-T cells targeting CD19/BCMA in multiple myeloma have shown promising patient responses in small-scale studies. TCR-modified T cells directed against tumor-specific antigens have induced cancer regression in melanoma patients and reduced metastases in synovial cell sarcoma patients. TILs and LAK cells have also led to tumor regression in metastatic cancer patients, with LAK cells improving survival in melanoma and glioblastoma patients and TILs increasing objective clinical response rates in metastatic melanoma patients. CIK cells have reduced disease recurrence and improved overall survival in hepatocellular carcinoma and renal cell carcinoma patients, mainly through perforin-mediated tumor killing. However, γδ T cells, another subset of ACT, have yielded mixed results, with some studies indicating their suppressive nature and association with negative outcomes within the tumor microenvironment. Allogeneic NK cells, in ACT, have provided modest benefits in acute myeloid leukemia, ovarian cancer, and breast cancer patients due to inhibition by host Tregs and the tumor, along with high IL-2 toxicity.
In combined cell therapy approaches, CIK cells and tumor lysate-pulsed DCs have significantly prolonged median survival and improved overall survival and quality of life in colorectal cancer patients. Similarly, DC-CIK immunotherapy has extended overall survival and enhanced the quality of life in advanced non-small cell lung cancer patients. Combining tumor lysate-loaded DC and TIL immunotherapy has shown potential with objective clinical responses in advanced melanoma patients. TCR-modified T cells targeting melanoma-associated antigen recognized by T cells (MART-1) in conjunction with DCs have been effective against melanoma.
While less well-documented than ACT products, genetically engineered Mesenchymal Stem Cells (MSCs) have been explored in cancer treatment due to their tumor tropism and anti-tumorigenic properties. However, patient-administered MSCs have yet to show significant benefits, possibly due to inadequate cell homing to tumors or paradoxical pro-tumorigenic potential observed in preclinical studies. Notably, the first-in-human clinical trial for Celyvir, an autologous MSC-based therapy carrying oncolytic adenoviruses, reported disease stabilization in pediatric neuroblastoma patients, paving the way for further exploration of bioengineered MSCs carrying oncolytic viruses in glioblastoma and ovarian carcinoma patients.
Several cancer stem cell (CSC)-targeting agents have been approved or are under investigation, with mechanisms involving CSC pathways. These treatments represent another promising avenue in cancer therapy.
Regenerative Medicine
Regenerative medicine employs a person’s own cells and growth factors to restore lost tissue function, effectively repairing damaged tissues. Within the realm of regenerative medicine, several cell therapies have gained FDA approval and are either established practices or commercially available.
These therapies include:
- Keratinocyte and fibroblast-derived skin substitutes for treating conditions like diabetic foot ulcers or burns.
- Products containing keratinocytes and fibroblasts are used to treat surgically created vascular wound beds in the oral cavity.
- Intradermal injections of fibroblasts to enhance the appearance of nasolabial fold wrinkles.
- Implants containing chondrocytes for the treatment of knee cartilage defects.
- Cord blood-derived hematopoietic stem cell (HSC) and hematopoietic progenitor cell products for addressing various disorders of the hematopoietic system, whether inherited, acquired, or arising from myeloablative treatment.
While these commercial cell therapies are effective in tissue repair, they have not yet achieved the ability to fully regenerate tissues. The clinical development process for such therapies can be challenging, often slowing down the introduction of new products to the market. This is evident in the statistics, where only 23% of all approved drugs over a nine-year period were biologics. Additionally, biologics in the United States enjoy 12 years of exclusivity protection, as opposed to approximately 7 years for new chemical entities.
Immune System Disorders
Most immune system disorders arise from overactive immune responses or autoimmune attacks. The primary approach to treatment focuses on reducing inflammation, alleviating symptoms, and preventing relapses. However, there is growing interest in using cell therapy to reset the immune system as a potential long-term cure. Since the late 1990s, Bone Marrow Transplantation/Hematopoietic Stem Cell Transplantation (BMT/HSCT) has emerged as a prominent cell-based therapy for immune system disorders. HSCT has demonstrated lasting results in severe Sjögren’s syndrome (SS) with acceptable rates of transplant-related mortality. Controlled phase 2/3 trials have shown its effectiveness in autoimmune disorders, leading to significant improvements in disability status, disease relapse rates, MRI lesions, and quality of life for multiple sclerosis patients, with a 79% improvement in some cases. HSCT, including Peripheral Blood Stem Cell Transplantation (PBSCT), has also reduced disease activity and stabilized or reversed organ dysfunction in systemic lupus erythematosus (SLE) patients. While benefits in SLE are mainly reported through retrospective studies, prospective trials have not yielded significant advantages. However, HSCT has only shown transient or partial benefits in other immune diseases like rheumatoid arthritis (RA), vasculitis, and Crohn’s disease. Despite its widespread benefits in most immune system disorders, the exact mechanism of action for HSCT remains unclear, with non-specific benefits attributed to the accompanying lymphotoxic chemotherapy regimen that reduces autoreactive antibodies.
Mesenchymal Stem Cells (MSCs) have also demonstrated success in immune system disorders, specifically in graft-versus-host disease (GVHD), amyotrophic lateral sclerosis, and Crohn’s anal fistula. These benefits stem from the immunomodulatory actions of MSCs, primarily through their immune inhibitory secretome. While several MSC-based therapies are approved worldwide for treating immune diseases, they have not yet received FDA approval. Adipose-Derived Stem Cells (ADSCs), although less documented than Bone Marrow-Derived MSCs (BM-MSCs), hold promise for treating immune system disorders such as GVHD, Crohn’s disease, psoriasis, and Sjögren’s syndrome.
Other cell-based therapies with reported but lesser benefits in immune diseases include Platelet-Rich Plasma (PRP), which has shown pain and inflammation reduction, supported by ultrasound imaging evidence in rheumatoid arthritis (RA) patients. Regulatory T cells (Tregs) have been found to lower the incidence of acute GVHD. Dendritic Cells (DCs), particularly tolerogenic DCs that induce T-cell anergy and Treg differentiation, have stabilized disease or reduced inflammation and disease scores in RA patients.
Additional somatic cell-based therapies like pancreatic islet cell transplantation have delivered substantial benefits in type 1 diabetes. For instance, a single-arm phase 3 trial revealed that pancreatic islet transplantation leads to improved glycemic control and protection against severe hypoglycemic events in type 1 diabetes patients. Therefore, global recommendations now consider pancreatic islet transplantation for patients with persistent problematic hypoglycemia despite insulin infusion or glycemic monitoring. Notably, clinical outcomes in pancreatic islet cell transplantation correlate with islet availability and engraftment success rates, which are higher in allogeneic transplants where islets can be isolated from multiple donors.
However, immunotherapies like CAR-T cells have not yet demonstrated clinical benefits in immune conditions, despite promising preclinical results.
Regulatory Considerations
As a researcher or manufacturer working in the field of cell therapy, it is important to be aware of the regulatory guidance provided by the FDA. The FDA defines HCT/P (human cells, tissues, and cellular and tissue-based products) as “articles containing or consisting of human cells or tissues that are intended for implantation, transplantation, infusion, or transfer into a human recipient” under Title 21 of the Code of Federal Regulations Part 1271.3(d). If your therapy falls under this definition, it must comply with the regulations outlined in 21 CFR Part 1271.15(b) and 21 CFR 1271.10(a), which specify that the HCT/P must be minimally manipulated, intended for homologous use, not combined with other active agents, without a systemic effect, and administered autologously or to first-/second-degree blood relatives. If these criteria are met, the FDA allows the use of the cell therapy in the framework of regulatory guidelines governing disease transmission, yet without premarket approval/biologics license application, solely under section 361 of the Public Health Service (PHS) Act and regulations in 21 CFR Part 1271. However, if the therapy does not meet these criteria, it is regulated as a biological product under the Federal Food, Drug, and Cosmetic (FD&C) Act and/or section 351 of the PHS Act and applicable regulations, and would require premarket approval. Recent enforcement by the FDA against stem cell clinics has shown that it is important to fully understand and comply with these regulations to protect patients from risks associated with unapproved products.
To conclude, Cell therapy is an expanding global market encompassing stem cell- and non–stem cell-based unicellular and multicellular therapies, which largely differ in their characteristics, isolation sources, and areas of use. A multitude of cell therapies have either become established practices or received FDA approval for certain indications. Other investigational and premarket approval-exempt cellular therapies have achieved a highly reputable track record in clinical settings, providing significant benefits to patients with degenerative disorders, immune diseases, and cancer. However, the clinical application of cell therapies in areas like neurodegenerative diseases still needs to bypass several issues, including the standardization of cell manufacturing methods and the slow disease progression rendering clinical outcomes hard to measure. Other hurdles limiting the advancement of cell therapies are related to safety, which with certain products like CAR-T cells could pose life-threatening toxicities. Limited clinical indications, high production costs, and high patient costs are other issues associated with cell therapies that need to be addressed by ongoing and future clinical trials. On another note, recent investigations have surfaced a partially supported notion that a mixture of cell types, such as SVF or BMAC, more closely mimics physiological interactions and could thus be more important than a single cell type, such as ADSCs or MSCs, in regenerative medicine and cancer treatment. Although more comparative studies are required to strengthen the quality of current evidence about their possible therapeutic superiority, multicellular therapies present with other advantages over unicellular therapies, including their lower cost and greater potential for exploitation by currently advancing gene engineering technologies and bioinformatic tools as a bridge to precision medicine.